In this article, you will learn:
- The TRUTH about glucose and how to know if you’re getting enough or too little
- 8 tips to optimise blood glucose level
- Tips to manage insulin resistance
- And much more…
How Does The Body Assimilate Glucose Molecules?
Your body either:
- Utilises glucose for energy
- Or stores glucose for future use
More specifically, one of these 4 things happen in the body:
- The body burns glucose for energy by synthesizing adenosine triphosphate (ATP)
- The body stores glucose in the liver
- The body stores glucose in the muscle tissue
- The glucose becomes body fat via gluconeogenesis
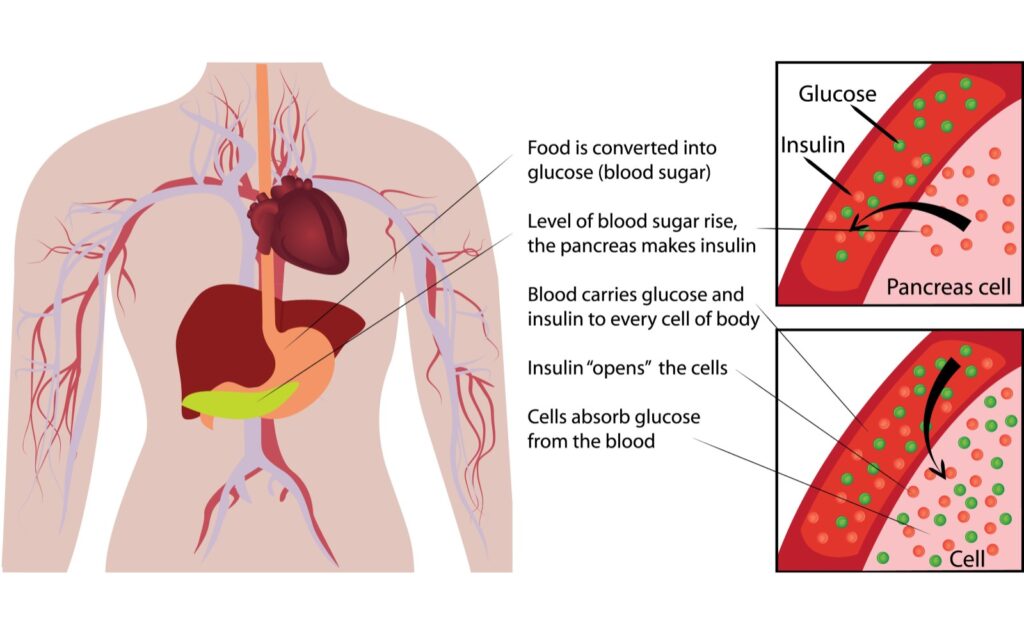
One of the keys to avoiding health problems and minimizing body fat gain is keeping a high level of insulin sensitivity.
Managing blood sugar levels is one of the best ways to BiOptimize this. If your fasted blood sugar creeps up too much, you should start taking steps to lower this.
Ideally, your fasted blood sugar is between 80-94. 100 to 125 is considered suboptimal. If it’s 126 on two different tests, it’s a good idea to consult a healthcare provider to rule out diabetes.
Some Simple Tips For Managing Blood Sugar And Insulin Resistance:
Take A 10-Minute Walk After Each Meal
[1][2][3][4][5]
Regular physical exercise is a mainstay for optimising blood glucose levels. The blood sugar levels in type 2 diabetics are significantly lower when they walk for 10 minutes after each meal. Credit goes to Stan Efferding for bringing awareness to this simple, powerful tip.
Intermittent sessions of moderate-intensity walking postmeal (preferably 30 minutes post-meal) is an effective method for controlling blood sugar levels in the elderly. The former is more effective than the standard 30- 45 minutes of continuous moderate-intensity walking.

30 minutes after a meal is when absorption happens, and glucose is the main fuel source. Therefore, exercising at that time maximizes the oxidation of glucose and uptake of glucose by contracting the muscles for energy.
Physical activity also improves insulin sensitivity in normal people and people with insulin resistance. A single physical activity session can raise insulin sensitivity for a minimum of 16 hours after exercise. The latter happens in both healthy people and people with type 2 diabetes.
Exercise reduces the glycogen stored in muscles. The latter improves insulin sensitivity, resulting in increased transport and utilization of glucose for energy.
Get Great Sleep
[6][7][8][9][10][11][12][13][14]
A good night’s sleep is vital in optimising blood glucose levels. Reduced sleep increases your risk of developing increased blood glucose. Studies suggest that sleep deprivation, even for one night, can reduce insulin sensitivity in healthy people. Sleep deprivation can therefore induce insulin resistance and affect blood sugar levels.
Therefore, not getting enough sleep can increase your risk of unstable blood sugar levels. The factors that affect the relationship between blood glucose level and sleep include:
- Age
- The total time you sleep
- The sleep stages you experience
- The time of the day you sleep
- Your eating habits
The physiological factors caused by reduced sleep that can increase blood sugar levels are:
- Sleep deprivation increases the hormone cortisol, which increases glucose levels
- Sleep deprivation reduces insulin sensitivity, thereby, impacting blood sugar levels
- Sleep deprivation increases poor inflammation and stress response, both of which impacts blood sugar levels
- The time of the day you sleep can impact cortisol and insulin levels, and both of these affect glucose levels
- Poor sleep increases C-reactive protein, which can affect blood sugar levels
Eat Lower Glycemic Carbohydrates
[15]
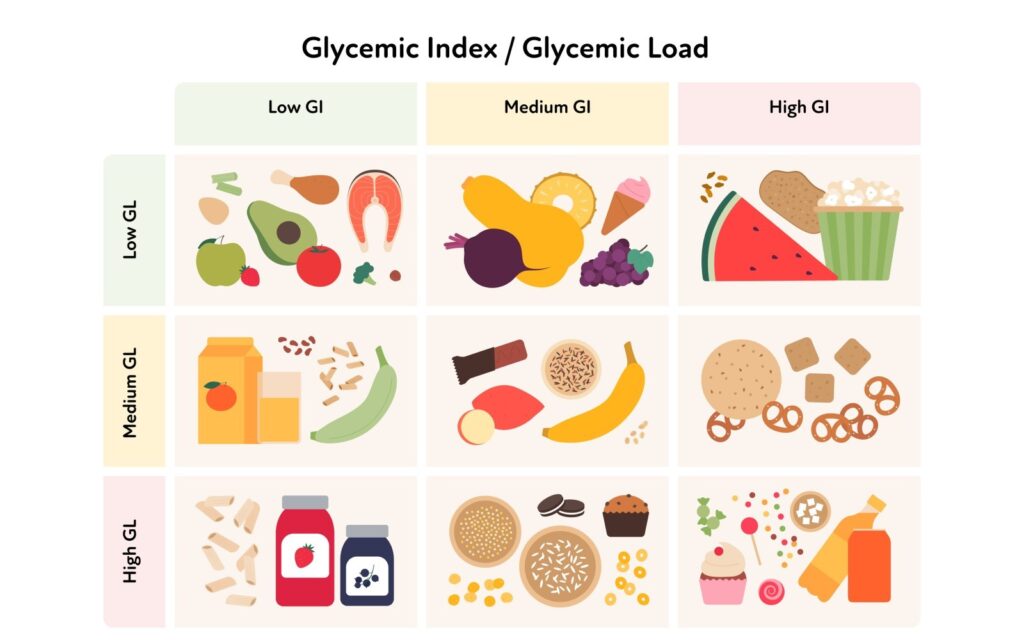
The Glycemic Index (GI) of food (carbohydrates) is the change in the blood sugar the food causes about a reference food. The reference food is generally white bread or glucose. Pure glucose has a glycemic index of 100. There are three types of glycemic index ratings:
- Low GI foods: 55 or less
- Medium GI foods: 56 to 69
- High GI foods: 70 or above
Your body digests and absorbs high-GI foods quickly. The latter, therefore, rapidly increases blood sugar levels. In contrast, your body breaks down and assimilates the low-GI foods (carbohydrates) slowly. The impact of low GI foods on insulin response and blood sugar levels is slower.
Therefore, eating lower glycemic carbohydrates is one of the best ways to manage your blood sugar levels. Studies show that low-GI diets effectively control fasting blood glucose in people with type 2 diabetes.
Some low-glycemic carbohydrate foods are:
- Vegetables
- Fruits
- Whole grains
- Legumes, lentils
- Dairy products
- Oats
Lower Daily Carb Intake
[16]
According to studies, a low-carb diet is one of the best ways to optimize blood glucose levels. A low-carb diet even helps treat both type 1 and type 2 diabetes.
According to the definition by the American Diabetes Association (ADA), a low-carb diet is when you get less than 130 g of carbs per day. This is less than 26 percent of your total energy intake.
Restriction of dietary carbohydrates reduced blood glucose levels and HbA1c the most. Lowering your daily carb intake usually doesn’t require lowering the number of calories, so adherence to such diets is better.
If Extreme Measures Need To Be Taken, Eliminate Carbs For A Few Weeks
[2][3]

Studies indicate that carb restriction for some time can effectively help with blood sugar levels. Very low-carb diets can induce a state of ketosis in your body. The latter is a metabolic process in which the body uses fat and ketones instead of sugar as the main energy source.
A very low-carb or ketogenic diet recommends 30 grams or fewer carbs per day. This is without any restriction on total calories.
Ketosis typically occurs when your daily intake of total carbs is less than 50 grams. You can significantly optimize blood glucose levels by restricting your carb intake to between 20 and 50 grams per day. This is especially true if you have diabetes.
Add Magnesium To Your Supplement Stack
[4][17][18]
People with poor blood sugar response tend to have low magnesium levels. This is because they don’t get enough magnesium from food and poor blood sugar response causes them to lose more magnesium in their urine.
Conversely, magnesium deficiency worsens everything because the magnesium inside your cells influences insulin activity and glucose uptake.
Therefore, magnesium supplementation can support healthy insulin response by replenishing body magnesium levels.
Add Spices To Your Diet: Specifically Curcumin, Ginger, Garlic, Cinnamon And Fenugreek
[19][20][21][22][23]

Many herbs and spices regulate blood sugar levels. Some of these include:
- Curcumin present in turmeric
- Ginger
- Garlic
- Ceylon Cinnamon
- Fenugreek
Curcumin is the spice turmeric’s bioactive compound used in Indian curries. It possesses powerful inflammation-balancing and antioxidant properties. Curcumin supports a healthy blood sugar response and counteracts oxidative stress from high blood sugar. It works by suppressing glucose production from proteins and fats in the liver.
Garlic also reduces blood sugar in animal studies.
Gingerol, an active compound in ginger, improves glucose uptake by muscle cells. Therefore, ginger can support healthy blood sugar control.
Fenugreek seeds also help balance blood sugar and support healthy insulin response.
A compound present in cinnamon, called Ceylon, mimics insulin. Cinnamon also promotes healthy blood sugar levels by making the cells more sensitive to insulin.
Do Cold Therapy: Cryotherapy Or Cold Baths
[1][24][25][26][27][28][29][30][31]

Cold baths and cryotherapy can improve blood sugar response and glucose metabolism by:
- Shivering of skeletal muscles
- Stimulation of heat-producing processes
Exposure to cold increases energy expenditure due to shivering and heat production. The latter is fueled by raised utilization of carbohydrates, proteins and fats. All these lead to a reduction in circulating blood sugar levels.
Studies also show that cold exposure improves glucose tolerance. Therefore, if you track your blood sugar, you’ll see a rapid drop in your blood sugar after a cold bath.
Supplement To Promote Healthy Blood Sugar Levels
We’ve created a very special formula to help promote healthy blood sugar levels. It’s called Berberine Breakthrough. This formula is a synergistic blend of science-backed ingredients to control blood sugar at clinically effective doses. Berberine Breakthrough helps to:
- Support healthy insulin response
- Improve carbohydrate metabolism
- Increase uptake of blood glucose by muscles
- Promote healthy blood sugar levels
Magnesium Breakthrough is the best magnesium supplement out there, with 7 different forms of highly-absorbed magnesium.
- Reynolds AN, Mann JI, Williams S, Venn BJ. Advice to walk after meals is more effective for lowering postprandial glycaemia in type 2 diabetes mellitus than advice that does not specify timing: a randomised crossover study. Diabetologia. 2016;59(12):2572-2578. doi:10.1007/s00125-016-4085-2
- Holmäng A, Björntorp P. The effects of cortisol on insulin sensitivity in muscle. Acta Physiol Scand. 1992;144(4):425-431. doi:10.1111/j.1748-1716.1992.tb09316.x
- Adam TC, Hasson RE, Ventura EE, et al. Cortisol is negatively associated with insulin sensitivity in overweight Latino youth. J Clin Endocrinol Metab. 2010;95(10):4729-4735. doi:10.1210/jc.2010-0322
- de Lordes Lima M, Cruz T, Pousada JC, Rodrigues LE, Barbosa K, Canguçu V. The effect of magnesium supplementation in increasing doses on the control of type 2 diabetes. Diabetes Care. 1998;21(5):682-686. doi:10.2337/diacare.21.5.682
- DiPietro L, Gribok A, Stevens MS, Hamm LF, Rumpler W. Three 15-min bouts of moderate postmeal walking significantly improves 24-h glycemic control in older people at risk for impaired glucose tolerance. Diabetes Care. 2013;36(10):3262-3268. doi:10.2337/dc13-0084
- González-Ortiz M, Martínez-Abundis E, Balcázar-Muñoz BR, Pascoe-González S. Effect of sleep deprivation on insulin sensitivity and cortisol concentration in healthy subjects. Diabetes Nutr Metab. 2000;13(2):80-83.
- Donga E, van Dijk M, van Dijk JG, et al. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010;95(6):2963-2968. doi:10.1210/jc.2009-2430
- Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and Type 2 diabetes. J Appl Physiol. 2005;99(5):2008-2019. doi:10.1152/japplphysiol.00660.2005
- Rains JL, Jain SK. Oxidative stress, insulin signaling, and diabetes. Free Radic Biol Med. 2011;50(5):567-575. doi:10.1016/j.freeradbiomed.2010.12.006
- Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105(3):1044-1049. doi:10.1073/pnas.0706446105
- Reutrakul S, Hood MM, Crowley SJ, et al. Chronotype is independently associated with glycemic control in type 2 diabetes. Diabetes Care. 2013;36(9):2523-2529. doi:10.2337/dc12-2697
- Frank SA, Roland DC, Sturis J, et al. Effects of aging on glucose regulation during wakefulness and sleep. Am J Physiol. 1995;269(6 Pt 1):E1006-16. doi:10.1152/ajpendo.1995.269.6.E1006
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. doi:10.1016/S0140-6736(99)01376-8
- Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43(4):678-683. doi:10.1016/j.jacc.2003.07.050
- Ojo O, Ojo O, Adebowale F, Wang XH. The effect of dietary glycaemic index on glycaemia in patients with type 2 diabetes: A systematic review and meta-analysis of randomized controlled trials. Nutrients. 2018;10(3):373. doi:10.3390/nu10030373
- Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015;31(1):1-13. doi:10.1016/j.nut.2014.06.011
- Morais JBS, Severo JS, de Alencar GRR, et al. Effect of magnesium supplementation on insulin resistance in humans: A systematic review. Nutrition. 2017;38:54-60. doi:10.1016/j.nut.2017.01.009
- Barbagallo M, Dominguez LJ. Magnesium and type 2 diabetes. World J Diabetes. 2015;6(10):1152-1157. doi:10.4239/wjd.v6.i10.1152
- Kim T, Davis J, Zhang AJ, He X, Mathews ST. Curcumin activates AMPK and suppresses gluconeogenic gene expression in hepatoma cells. Biochem Biophys Res Commun. 2009;388(2):377-382. doi:10.1016/j.bbrc.2009.08.018
- Jalal R, Bagheri SM, Moghimi A, Rasuli MB. Hypoglycemic effect of aqueous shallot and garlic extracts in rats with fructose-induced insulin resistance. J Clin Biochem Nutr. 2007;41(3):218-223. doi:10.3164/jcbn.2007031
- Li Y, Tran VH, Duke CC, Roufogalis BD. Gingerols of Zingiber officinale enhance glucose uptake by increasing cell surface GLUT4 in cultured L6 myotubes. Planta Med. 2012;78(14):1549-1555. doi:10.1055/s-0032-1315041
- Jarvill-Taylor KJ, Anderson RA, Graves DJ. A hydroxychalcone derived from cinnamon functions as a mimetic for insulin in 3T3-L1 adipocytes. J Am Coll Nutr. 2001;20(4):327-336. doi:10.1080/07315724.2001.10719053
- Gupta A, Gupta R, Lal B. Effect of Trigonella foenum-graecum (fenugreek) seeds on glycaemic control and insulin resistance in type 2 diabetes mellitus: a double blind placebo controlled study. J Assoc Physicians India. 2001;49:1057-1061. Accessed July 7, 2022. https://pubmed.ncbi.nlm.nih.gov/11868855/
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717. doi:10.1016/j.metabol.2008.01.013
- Pang B, Zhao LH, Zhou Q, et al. Application of berberine on treating type 2 diabetes mellitus. Int J Endocrinol. 2015;2015:905749. doi:10.1155/2015/905749
- Dong H, Wang N, Zhao L, Lu F. Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis. Evid Based Complement Alternat Med. 2012;2012:591654. doi:10.1155/2012/591654
- Ivanova YM, Blondin DP. Examining the benefits of cold exposure as a therapeutic strategy for obesity and type 2 diabetes. J Appl Physiol. 2021;130(5):1448-1459. doi:10.1152/japplphysiol.00934.2020
- Murday AJ, Gershlick AH, Syndercombe-Court YD, Mills PG, Lewis CT. Intimal thickening in autogenous vein grafts in rabbits: influence of aspirin and dipyridamole. Thorax. 1984;39(6):457-461. doi:10.1136/thx.39.6.457
- Murdoch C, Unwin D, Cavan D, Cucuzzella M, Patel M. Adapting diabetes medication for low carbohydrate management of type 2 diabetes: a practical guide. Br J Gen Pract. 2019;69(684):360-361. doi:10.3399/bjgp19X704525
- Snorgaard O, Poulsen GM, Andersen HK, Astrup A. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2017;5(1):e000354. doi:10.1136/bmjdrc-2016-000354
- Cucuzzella M, Riley K, Isaacs D. Adapting medication for Type 2 diabetes to a low carbohydrate diet. Front Nutr. 2021;8:688540. doi:10.3389/fnut.2021.688540